Home » Blog » Methylene Blue » Methylene blue for treating Methemoglobinemia
Table of Contents
What is Methemoglobinemia?
Methemoglobinemia is a blood disease in which there is an oxygen deficiency in the cells. Haemoglobin, a protein linked to red blood cells, transports oxygen through the circulation. Normally, haemoglobin then transports oxygen to cells all over the body. However, methemoglobin is a form of haemoglobin that transports oxygen through the blood but does not release it into the cells. When your body creates an excessive amount of methemoglobin, it begins to replace the regular haemoglobin. This can result in insufficient oxygen reaching the cells. Common symptoms associated with methemoglobinemia are cyanosis (bluish colour of the skin, especially the lips and fingers), headache, dizziness, shortness of breath, nausea, and poor muscle coordination. Serious symptoms include central nervous system depression, metabolic acidosis, seizures, dysrhythmias, coma, and death.
Methylene Blue Injection is used in the treatment of methemoglobinemia, this article will shed light on how methylene blue works in treating this disease.
Before we delve into methylene blue and its treatment we will discuss a bit more about methemoglobinemia. The symptoms of methemoglobinemia differ based on the kind. Methemoglobinemia is classified into two types: acquired and congenital.
Genetic or Congenital
Methemoglobinemia can be congenital, which means that the person is born with it. Congenital methemoglobinemia is caused by a genetic flaw passed down from the parents. This genetic flaw causes a lack of a certain enzyme or protein. This protein is in charge of converting methemoglobin into haemoglobin. Congenital methemoglobinemia is far less frequent than acquired methemoglobinemia.
Congenital methemoglobinemia is classified into three categories.
TYPE 1 – The most frequent form of congenital methemoglobinemia is type 1. It happens when both parents have the gene but do not have the disease themselves. It exclusively affects red blood cells. The only sign is usually cyanosis. People with type 1 diabetes can have bluish-tinted skin their whole lives without experiencing any additional symptoms. They might be treated for aesthetic purposes. People of this kind are more likely to develop acquired forms.
Haemoglobin M Disease – This kind is caused by a genetic mutation that you may or may not inherit from your parents. This kind has no symptoms and does not require treatment.
TYPE 2 – Cytochrome b5 reductase deficiency is another name for type 2. It is the most uncommon kind of methemoglobinemia. Type 2 affects every cell in the body. The faulty gene just has to be passed down from one of your parents. It can result in serious developmental issues and the inability to thrive. Babies who are born with type 2 diabetes generally die within the first year.
Acquired
This is also referred to as acute methemoglobinemia. The most frequent form of methemoglobinemia is acquired methemoglobinemia. It is caused by the ingestion of certain drugs, chemicals, or foods. People who have a hereditary version of the disease are more likely to develop the acquired kind. However, the majority of persons who develop this illness do not have a congenital issue. If acquired methemoglobinemia is not treated promptly, it can be fatal. Babies are the most vulnerable to this disease. Babies can develop acquired methemoglobinemia from causes such as consumption of Bencozaine, polluted well water and solid meals.
Adults usually get acquired methemoglobinemia after undergoing medical procedures that employ topical anaesthetics, which are often administered on the skin. Among them are benzocaine, lidocaine, and prilocaine.
How does methylene blue work?
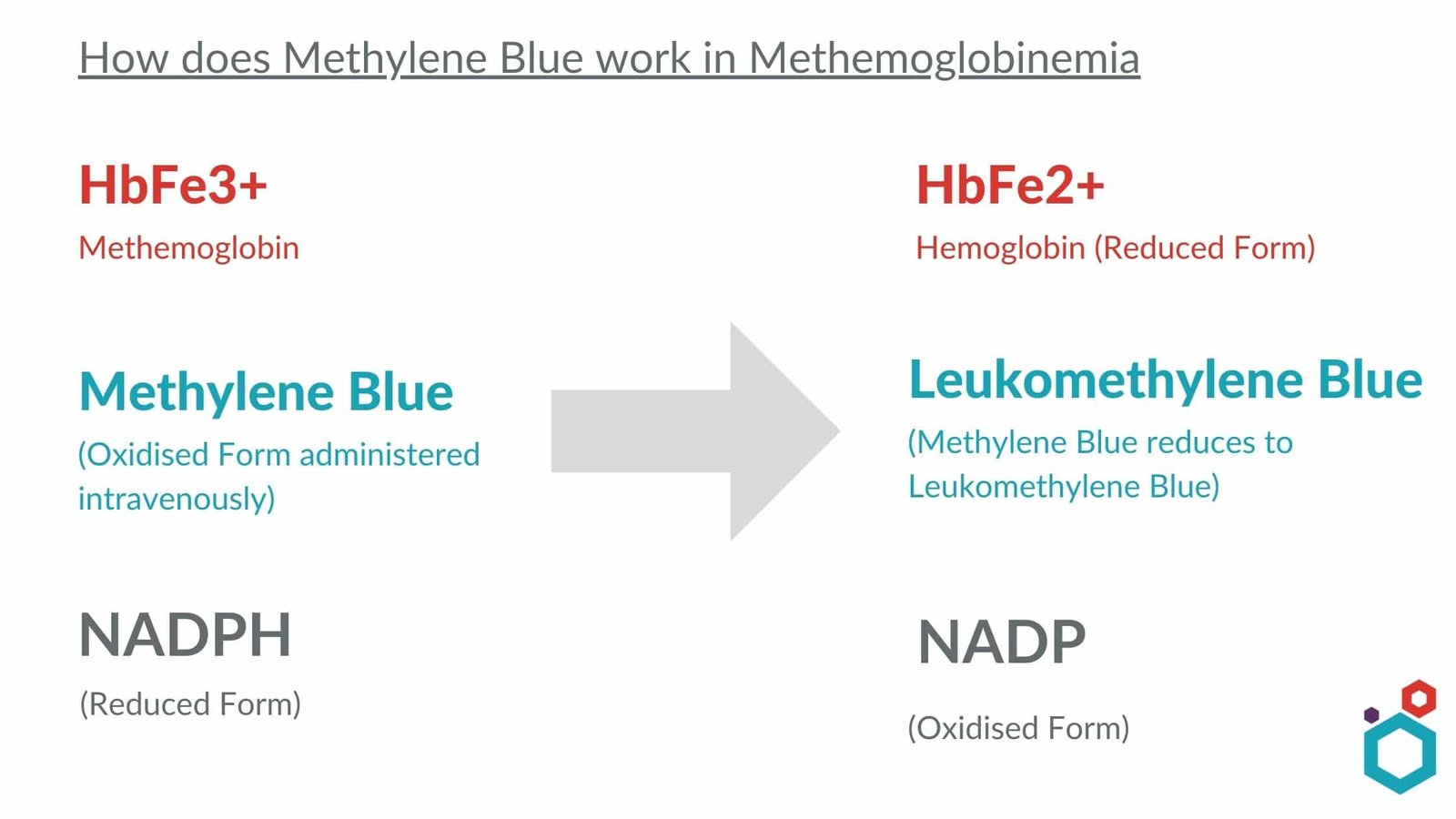
Methylene Blue is known for its oxidizing properties, and it is because of this trait that it works as a treatment for Methemoglobinemia. Methylene Blue oxidizes NADPH and turns into Leukomethylene Blue. Leukomethylene Blue then oxidizes methemoglobin and converts it into haemoglobin. . Methylene blue returns haemoglobin’s iron to its natural (reduced) oxygen-carrying condition. This is accomplished by supplying a fictitious electron acceptor
Methylene Blue treatment will not work for those with glucose-6-phosphate dehydrogenase (G6PD) deficiency as G6PD is a crucial compound for generating NADPH, and in absence of sufficient NADPH, the administered methylene blue will not be able to convert or reduce into leukomethylene blue. Excess of unreduced methylene blue can oxidise haemoglobin itself, creating more methemoglobin.
How is Methylene Blue treatment administered?
Prompt identification of the disease and treatment start, when warranted (particularly in acquired methemoglobinemia), are important in methemoglobinemia therapy. At the same time, it may be necessary to begin comprehensive, often invasive, tests to rule out cardiac and pulmonary problems, which frequently result in a clinical presentation similar to cyanosis.
Through an IV, methylene blue USP is administered into a vein. This injection will be administered by a healthcare practitioner. It may take up to 30 minutes to complete the IV infusion. It is administered in a 1-2 mg/kg dosage as a 1% solution in IV saline over 3-5 minutes. Although the reaction is typically quick, if the level of methemoglobin is still high one hour after the initial infusion, the dosage may be repeated in one hour.
While you are getting methylene blue, your respiration, blood pressure, oxygen levels, renal function, and other vital indicators will be continuously monitored. Your blood will also be checked to assist your doctor to evaluate whether the medication is working.
You might just need one dosage of methylene blue. If you require a second dose, it can be given one hour after the first.
Methylene blue will almost certainly turn urine or faces blue or green in hue. This is a common side effect of the medicine and will have no negative consequences. This impact, however, may provide unexpected findings with some urine tests.
Initial treatment consists of administering supplemental oxygen and removing the problematic oxidizing chemical. The first-line antidote is intravenous (IV) methylene blue. Following MB therapy, it is acceptable to do repeated assessments of MetHb levels. Patients with glucose 6-phosphate dehydrogenase (G6PD) impairment should not be given MB since the lowering of MetHb by MB is dependent on NADPH produced by G6PD (hemolysis). Ascorbic acid (2mg/kg) is an alternate therapy for these individuals.
For patients with severe methemoglobinemia who do not react to or can’t be treated with methylene blue, exchange transfusion and hyperbaric oxygen therapy are second-line alternatives.
FAQs
Q. What should you avoid if you are given methylene blue?
- Methylene blue may cause impaired vision and interfere with your thoughts or reflexes. If you drive or do anything else that requires you to be attentive and able to see well, be cautious.
- Avoid exposure to sunshine or tanning beds for at least 24 hours following methylene blue therapy. This medication may make you more susceptible to sunburn. When going outside, use protective clothing and apply sunscreen (SPF 30 or higher).
Q. What is methemoglobin (MetHb)?
Methemoglobin is a defective type of haemoglobin. In methemoglobin, the iron in the heme group is in the Fe3+ state, as opposed to the Fe2+ state that is present in normal haemoglobin. Because it is unable to bind oxygen, it is also unable to transport oxygen, which lowers the amount of oxygen in the circulation and has the potential to induce hypoxemia in the tissues.
Q. What is the dose of methylene blue for methemoglobinemia?
The usual adult dose for Methemoglobinemia is as follows:
Drug-Induced Methemoglobinemia:
Methylene blue injection 1%: 0.1 to 0.2 mL/kg IV very slowly over a period of several minutes; may repeat in one hour if necessary
Acquired Methemoglobinemia:
Methylene blue injection 0.5% [Provayblue (TM)]: 1 mg/kg IV over 5 to 30 minutes; if the methemoglobin level remains greater than 30% or if symptoms persist, a repeat dose of 1 mg/kg IV may be given one hour after the first dose; if methemoglobinemia does not resolve after 2 doses, consider alternative interventions
Q. Can methylene blue cause methemoglobinemia?
Methylene blue is an oxidizing agent at doses greater than 7 mg/kg. Thus, it may cause methemoglobinemia in susceptible patients by oxidizing haemoglobin at higher concentrations.
Q. What is the cure for methemoglobinemia?
Methylene blue is the principal treatment for methemoglobinemia in patients who have documented symptoms of the condition. It is administered intravenously as a 1 percent solution in saline over the course of three to five minutes at a dose of 1-2 mg/kg (up to a total of 50 mg in adults, adolescents, and older children).
Q. What is the antidote for methemoglobinemia?
Methylene blue is the first-line therapy for symptomatic methemoglobinemia. Alternative treatments, such as ascorbic acid and hyperbaric oxygen, can be effective when methylene blue cannot be obtained.
Q. What is the cause of methemoglobinemia?
Methemoglobinemia can be acquired or congenital. Acquired methemoglobinemia is caused by exposure to certain medicines, chemicals, or foods. Congenital methemoglobinemia is caused by a genetic defect that you inherit from your parents. This genetic defect leads to cytochrome b5 reductase enzyme deficiency (type I b5R).
Q. What is the treatment for methemoglobinemia for those with G6PD deficiency?
Methylene blue is contraindicated in G6PD deficiency. In these specific cases, moderate doses of ascorbic acid (300 to 1,000 mg/day orally in divided doses) should be given.
Disclaimer-
The information provided here is based on general knowledge, articles, research publications etc and we do not claim the authenticity of any of the information provided above. We do not claim or suggest/advise any medical, therapeutic, health or nutritional benefits of MB. We do not supply or promote our MB product for the applications which are covered by valid patents and which are not approved by the FDA.
Macsen Labs is a manufacturer and supplier of several grades of Methylene Blue such as:-
- Methylene Blue USP
- Methylene Blue Zinc Free
- Methylene Blue BP 2000
- Methylene Blue BP 1973
- Methylthioninium Chloride BP
- Methylthioninium Chloride EP 9.0
- Methylthioninium Chloride E.P-10
Macsen Labs group’s Methylene Blue Synthesis Process granted a patent from the Indian patent office
The Indian Patent Office granted a patent to Mr Achal Agrawal, CEO of Macsen Labs, Udaipur. The title of the patent is Novel Improved Method for Synthesis of Diaminophenothiazine Compounds and it concerns a novel process for synthesising the compound Methylthioninium Chloride or Methylene Blue. Macsen Labs has now achieved a unique position by this patent and from now nobody will be able to copy this process. Read more
Read our other articles here
- Methylene Blue Dye | Chemistry, Uses & Side effects
- Staining with Methylene Blue
- Methylene Blue’s uses in Fish Aquaculture
- Methylene Blue Injection: Indications, Dosage & Brands
- Methylene Blue in the treatment of Alzheimer’s
- Methylene Blue in Covid-19
- Methylene Blue Against Cyanide Poisoning
- Malaria Treatment with Methylene Blue
- Methylene Blue treatment for Lumpy Skin disease in cattle
- Methylene Blue for Cancer Therapy


